Delving into the realm of bariatric surgery, this comprehensive guide explores which statement accurately describes bariatric surgery options, unraveling the complexities of this transformative medical intervention. With a focus on evidence-based information and expert insights, this discourse aims to empower individuals seeking a deeper understanding of their weight loss journey.
Bariatric surgery encompasses a spectrum of procedures designed to address severe obesity and its associated health risks. Understanding the mechanisms of action, patient selection criteria, surgical techniques, and post-operative care protocols is paramount for informed decision-making. This guide delves into each aspect, providing a thorough examination of bariatric surgery options and their implications.
Types of Bariatric Surgery
Bariatric surgery encompasses a range of surgical procedures aimed at reducing weight and improving health outcomes in individuals with severe obesity. These procedures can be broadly classified into three main categories:
- Restrictive procedures: These surgeries limit the amount of food that can be consumed by altering the anatomy of the stomach. Examples include sleeve gastrectomy and gastric banding.
- Malabsorptive procedures: These surgeries bypass a portion of the digestive tract, reducing the absorption of nutrients. Examples include Roux-en-Y gastric bypass and biliopancreatic diversion with duodenal switch.
- Combined procedures: These surgeries combine elements of both restrictive and malabsorptive procedures, such as sleeve gastrectomy with duodenal switch.
Mechanism of Action
Restrictive procedures: These surgeries reduce the size of the stomach, creating a smaller pouch that limits food intake. This leads to earlier satiety and reduced caloric consumption. Malabsorptive procedures: These surgeries bypass a portion of the small intestine, where most nutrients are absorbed.
This results in decreased absorption of calories and nutrients, leading to weight loss. Hormonal changes: Bariatric surgery can also induce hormonal changes that affect appetite and metabolism. These changes may include increased production of satiety hormones and decreased production of hunger hormones.
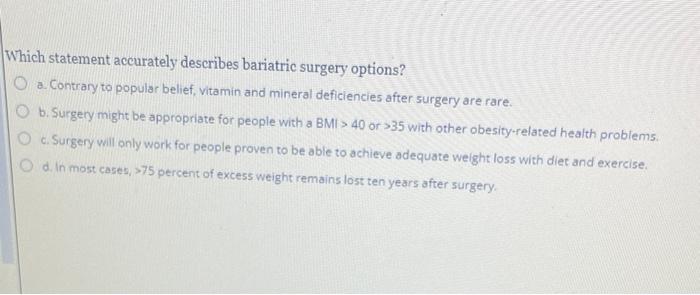
Patient Selection, Which statement accurately describes bariatric surgery options
Eligibility for bariatric surgery is typically determined based on several criteria, including:
- Body mass index (BMI) of 40 or higher, or a BMI of 35 or higher with significant comorbidities
- Failed attempts at non-surgical weight loss methods
- Absence of severe psychiatric disorders or active substance abuse
- Realistic expectations and commitment to lifestyle changes
Multidisciplinary teams, including surgeons, physicians, dietitians, and psychologists, evaluate patients to assess their suitability for bariatric surgery.
Surgical Techniques
Sleeve gastrectomy: This procedure involves removing a large portion of the stomach, leaving behind a narrow tube-like structure. Gastric banding: This procedure places an adjustable band around the upper part of the stomach, creating a smaller pouch and restricting food intake. Roux-en-Y gastric bypass: This procedure creates a small stomach pouch and connects it directly to the small intestine, bypassing a portion of the stomach and upper small intestine.
Biliopancreatic diversion with duodenal switch: This procedure involves removing a large portion of the stomach and bypassing most of the small intestine, leaving only a short segment connected to the large intestine.Each procedure carries its own risks and complications, which should be discussed thoroughly with the surgical team.
Post-Operative Care
After bariatric surgery, patients typically require a period of hospitalization for monitoring and recovery. Post-operative care includes:
- Dietary restrictions and modifications to gradually transition to a healthy eating plan
- Lifestyle changes, such as regular exercise and stress management
- Medical monitoring, including regular follow-up appointments and laboratory tests
Long-term follow-up and support are crucial for maintaining weight loss and preventing complications.
Q&A: Which Statement Accurately Describes Bariatric Surgery Options
What is the primary goal of bariatric surgery?
The primary goal of bariatric surgery is to achieve significant and sustained weight loss, thereby reducing the risks and complications associated with severe obesity.
What are the different types of bariatric surgery procedures?
Bariatric surgery procedures can be categorized into three main types: restrictive procedures (e.g., sleeve gastrectomy, gastric banding), malabsorptive procedures (e.g., Roux-en-Y gastric bypass, biliopancreatic diversion with duodenal switch), and combined procedures (e.g., sleeve gastrectomy with duodenal switch).
What factors are considered when determining patient eligibility for bariatric surgery?
Patient eligibility for bariatric surgery is typically determined based on factors such as body mass index (BMI), comorbidities, psychological readiness, and a history of unsuccessful weight loss attempts.